Your cart is currently empty!
Uterine Fibroid
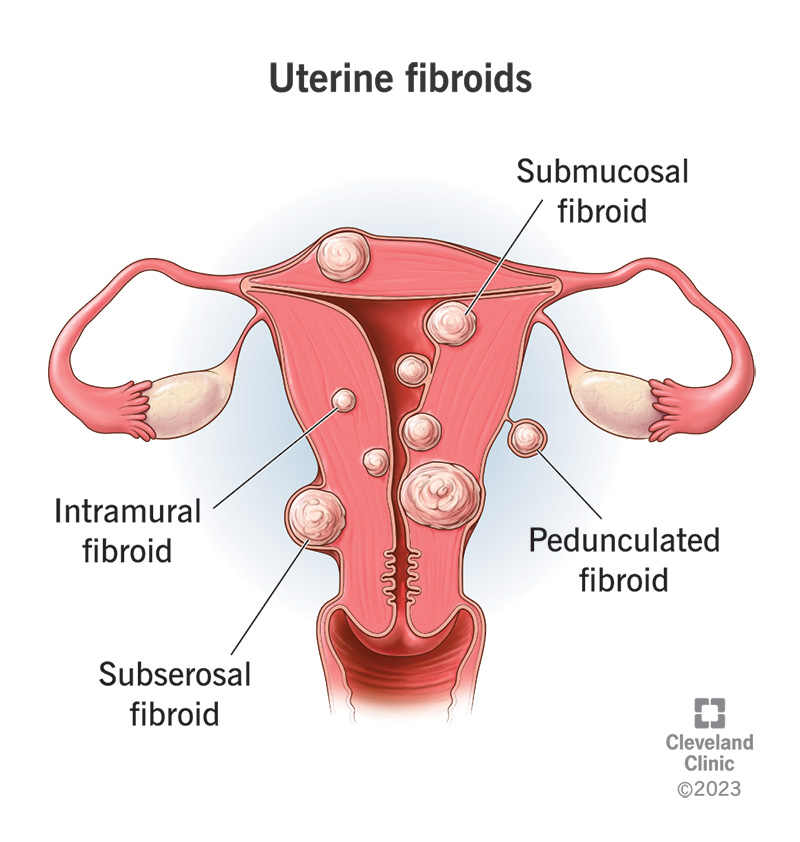
Uterine fibroids, also known as leiomyomas or myomas, are noncancerous growths that develop in the muscular wall of the uterus. They are the most common type of benign tumor found in the female reproductive system and can vary in size, number, and location within the uterus. While uterine fibroids are typically benign and do not increase the risk of uterine cancer, they can cause a range of symptoms and complications depending on their size and location.
Symptoms: The symptoms of uterine fibroids can vary widely among women and may include:
Heavy or Prolonged Menstrual Bleeding: Fibroids located near the uterine lining can cause heavy menstrual bleeding (menorrhagia) or prolonged periods.
Pelvic Pain or Pressure: Fibroids that grow large or press against nearby organs, such as the bladder or rectum, can cause pelvic pain, discomfort, or pressure.
Pelvic Discomfort: Some women may experience pelvic pain, discomfort, or a feeling of fullness or bloating, especially during menstruation or sexual intercourse.
Frequent Urination: Fibroids that press against the bladder can cause frequent urination or difficulty emptying the bladder completely.
Constipation or Difficulty With Bowel Movements: Fibroids that press against the rectum can cause constipation or difficulty with bowel movements.
Abdominal Enlargement or Swelling: Large fibroids or multiple fibroids may cause the uterus to enlarge, leading to a noticeable increase in abdominal girth or swelling.
Back or Leg Pain: Fibroids that press against nerves or blood vessels in the pelvis may cause back pain, leg pain, or sciatica-like symptoms.
Infertility or Pregnancy Complications: Depending on their size and location, fibroids can interfere with fertility or increase the risk of pregnancy complications, such as miscarriage, preterm birth, or breech presentation.
Causes: The exact cause of uterine fibroids is not fully understood, but several factors may contribute to their development, including:
Hormonal Factors: Estrogen and progesterone, hormones that regulate the menstrual cycle, may promote the growth of uterine fibroids. Fibroids tend to grow during reproductive years when hormone levels are high and typically shrink after menopause when hormone levels decline.
Genetic Factors: There may be a genetic predisposition to developing uterine fibroids, as they tend to run in families.
Other Factors: Other factors such as race (African-American women are at higher risk), obesity, diet, and lifestyle factors may also influence the development of uterine fibroids.
Diagnosis: Uterine fibroids are typically diagnosed through a combination of medical history, pelvic examination, and imaging tests, such as:
Ultrasound: Transvaginal ultrasound or abdominal ultrasound may be used to visualize the uterus and detect the presence, size, and location of fibroids.
Magnetic Resonance Imaging (MRI): MRI may be used to provide more detailed images of the uterus and fibroids, particularly for planning surgical procedures or evaluating large or complex fibroids.
Hysteroscopy or Hysterosalpingography (HSG): These procedures involve the insertion of a thin, flexible tube with a camera into the uterus (hysteroscopy) or the injection of contrast dye into the uterus followed by X-ray imaging (HSG) to evaluate the uterine cavity and detect abnormalities such as fibroids.
Treatment: Treatment for uterine fibroids depends on the severity of symptoms, the size and location of fibroids, and the woman’s reproductive plans. Treatment options may include:
Watchful Waiting: If fibroids are small, asymptomatic, or not causing significant problems, a “watchful waiting” approach may be recommended, with regular monitoring of symptoms and fibroid growth.
Medications: Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), hormonal contraceptives, gonadotropin-releasing hormone (GnRH) agonists, or selective progesterone receptor modulators (SPRMs) may be prescribed to manage symptoms such as heavy menstrual bleeding, pelvic pain, or pressure.
Minimally Invasive Procedures: Minimally invasive procedures, such as uterine artery embolization (UAE), myomectomy, or radiofrequency ablation (RFA), may be performed to shrink or remove fibroids while preserving the uterus and fertility.
Surgical Removal of Fibroids: Surgical procedures, such as myomectomy (surgical removal of fibroids) or hysterectomy (surgical removal of the uterus), may be recommended for women with severe symptoms, large or multiple fibroids, or who have completed childbearing and do not wish to preserve fertility.
Endometrial Ablation: Endometrial ablation may be considered for women with heavy menstrual bleeding who wish to avoid or delay more invasive surgical procedures. It involves the destruction or removal of the uterine lining to reduce menstrual bleeding.
Focused Ultrasound Surgery (FUS): Focused ultrasound surgery (FUS) is a noninvasive procedure that uses high-intensity ultrasound waves to heat and destroy fibroid tissue while leaving surrounding tissues unharmed.