Your cart is currently empty!
Sciatica
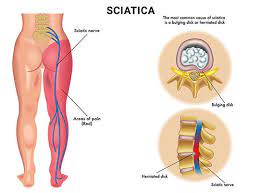
Sciatica refers to pain that radiates along the path of the sciatic nerve, which extends from the lower back through the hips and buttocks down each leg. It typically affects only one side of the body. Sciatica itself is not a medical condition but rather a symptom of an underlying problem affecting the sciatic nerve or its surrounding structures.
Causes of Sciatica:
Herniated Disc: A herniated or bulging disc in the lumbar spine (lower back) can compress or irritate the nearby sciatic nerve roots, leading to sciatica.
Degenerative Disc Disease: Degenerative changes in the spine, such as disc degeneration or spinal stenosis (narrowing of the spinal canal), can contribute to sciatica by putting pressure on the sciatic nerve.
Spinal Stenosis: Narrowing of the spinal canal in the lumbar spine due to bone spurs, herniated discs, or other degenerative changes can compress the sciatic nerve and cause symptoms of sciatica.
Piriformis Syndrome: The piriformis muscle, located deep in the buttocks, can sometimes irritate or compress the sciatic nerve, leading to symptoms similar to sciatica.
Spondylolisthesis: This condition occurs when one vertebra slips forward over an adjacent vertebra, potentially pinching the sciatic nerve roots as they exit the spine.
Trauma or Injury: Direct trauma to the lower back or buttocks, such as from a fall or motor vehicle accident, can injure the sciatic nerve and cause symptoms of sciatica.
Symptoms of Sciatica:
The most common symptom of sciatica is pain that radiates from the lower back or buttocks down the back of one leg. Other symptoms may include:
Pain: Sharp, shooting pain that radiates along the path of the sciatic nerve, often described as burning or electric-like pain. The pain may worsen with movement, prolonged sitting, or standing.
Numbness or Tingling: Numbness, tingling, or pins-and-needles sensations in the leg or foot, often following the path of the sciatic nerve.
Weakness: Weakness or difficulty moving the leg or foot, particularly when trying to lift the foot or toes.
Muscle Tightness: Muscle tightness or spasms in the lower back, buttocks, or leg, which may exacerbate symptoms.
Diagnosis and Treatment of Sciatica:
Diagnosis of sciatica typically involves a thorough medical history, physical examination, and diagnostic tests such as:
Imaging Studies: X-rays, MRI, or CT scans may be ordered to visualize the spine and identify any underlying structural abnormalities, such as herniated discs or spinal stenosis.
Electrodiagnostic Tests: Electromyography (EMG) or nerve conduction studies may be performed to assess the function of the sciatic nerve and determine the extent of nerve damage.
Treatment of sciatica depends on the underlying cause and severity of symptoms. Conservative treatment options may include:
Pain Medications: Over-the-counter or prescription medications such as NSAIDs (nonsteroidal anti-inflammatory drugs), muscle relaxants, or neuropathic pain medications may be prescribed to alleviate pain and inflammation.
Physical Therapy: Physical therapy exercises, stretches, and modalities such as heat or ice therapy may help relieve pain, improve flexibility, and strengthen the muscles supporting the spine.
Epidural Steroid Injections: Corticosteroid injections into the epidural space around the spinal nerves may be recommended to reduce inflammation and provide temporary pain relief.
Chiropractic Manipulation: Spinal manipulation performed by a qualified chiropractor may help alleviate symptoms of sciatica by improving spinal alignment and reducing nerve compression.
Acupuncture: Acupuncture, a traditional Chinese medicine technique involving the insertion of thin needles into specific points on the body, may help relieve pain and improve symptoms of sciatica for some individuals.
Surgery: In severe or refractory cases of sciatica that do not respond to conservative treatments, surgical interventions such as discectomy (removal of the herniated disc) or laminectomy (removal of bone spurs or part of the spinal canal) may be considered to decompress the affected nerves.