Your cart is currently empty!
Pneumonia
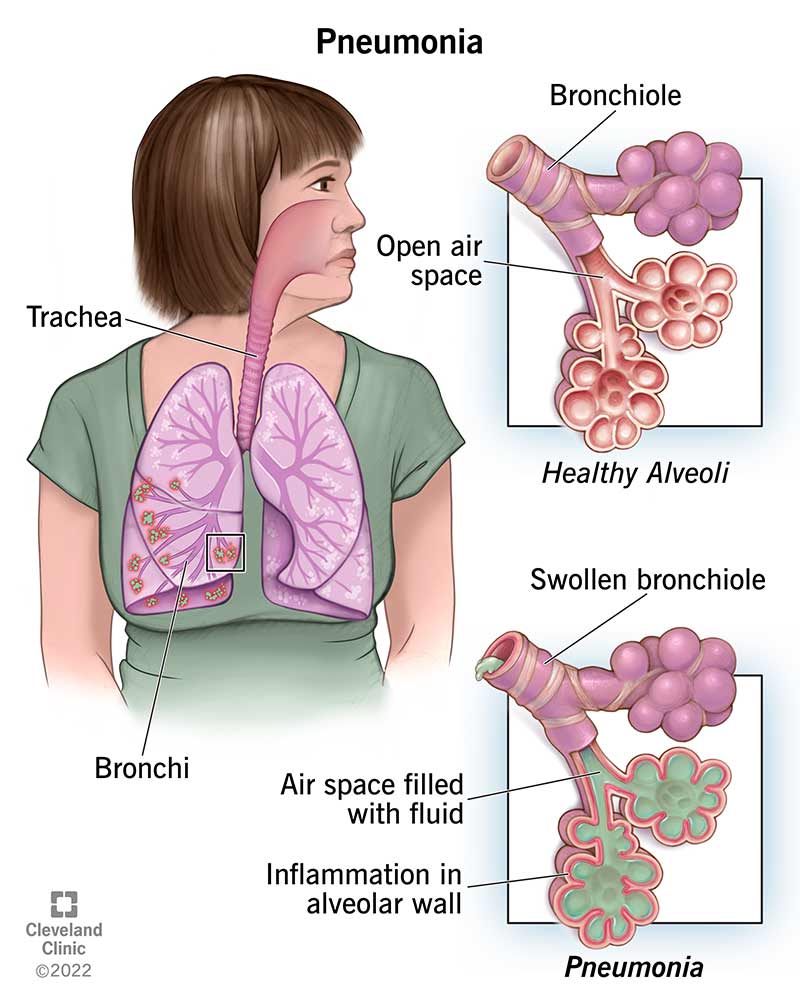
Pneumonia is an infection that inflames the air sacs in one or both lungs. The air sacs may fill with fluid or pus (purulent material), causing cough with phlegm or pus, fever, chills, and difficulty breathing. Pneumonia can range in severity from mild to life-threatening and can affect people of any age, but it is most dangerous in older adults, infants, and people with weakened immune systems.
Causes of Pneumonia:
Bacteria: The most common cause of bacterial pneumonia is Streptococcus pneumoniae. Other bacteria that can cause pneumonia include Haemophilus influenzae, Mycoplasma pneumoniae, Legionella pneumophila, and Staphylococcus aureus.
Viruses: Viral pneumonia is often caused by influenza viruses, respiratory syncytial virus (RSV), adenoviruses, or rhinoviruses. Viral pneumonia tends to be less severe than bacterial pneumonia but can still lead to serious complications, especially in vulnerable populations.
Fungi: Fungal pneumonia is less common and usually affects people with weakened immune systems, such as those with HIV/AIDS or individuals undergoing chemotherapy. Fungal organisms such as Pneumocystis jirovecii or Histoplasma capsulatum can cause pneumonia.
Aspiration: Aspiration pneumonia occurs when foreign material, such as food, drink, vomit, or saliva, is inhaled into the lungs, leading to inflammation and infection. This type of pneumonia is more common in people with swallowing difficulties, impaired consciousness, or conditions such as gastroesophageal reflux disease (GERD).
Symptoms of Pneumonia:
The symptoms of pneumonia can vary depending on the underlying cause, severity, and individual factors. Common symptoms may include:
Cough: Coughing that may produce phlegm or pus (sputum), which can be yellow, green, or bloody.
Fever: High fever, sweating, and chills, which may indicate an inflammatory response to infection.
Difficulty Breathing: Shortness of breath, rapid breathing, or wheezing, particularly with exertion or while lying down.
Chest Pain: Chest pain that worsens with deep breathing or coughing, due to inflammation of the lung tissue or pleura (lining of the chest cavity).
Fatigue: Generalized weakness, fatigue, or malaise, which may accompany fever or respiratory symptoms.
Nausea and Vomiting: Some individuals with pneumonia may experience nausea, vomiting, or gastrointestinal symptoms, particularly if the infection is severe or involves aspiration of gastric contents.
Confusion: Confusion, delirium, or changes in mental status, particularly in older adults or individuals with underlying medical conditions.
Other Symptoms: Other symptoms such as headache, muscle aches, sore throat, or loss of appetite may occur, depending on the underlying cause and individual factors.
Diagnosis and Treatment of Pneumonia:
Diagnosis of pneumonia typically involves a combination of medical history, physical examination, chest imaging studies, and laboratory tests. Diagnostic tests may include:
Chest X-ray: Imaging studies such as chest X-ray or chest CT scan may be ordered to visualize the lungs and assess for signs of pneumonia, such as infiltrates, consolidation, or pleural effusion.
Sputum Culture: Collection and analysis of sputum samples may be performed to identify the causative organism and guide antibiotic therapy in cases of bacterial pneumonia.
Blood Tests: Blood tests such as complete blood count (CBC), C-reactive protein (CRP), or procalcitonin levels may be measured to assess for signs of infection and inflammation.
Treatment of pneumonia depends on the underlying cause, severity of symptoms, and individual factors. Treatment options may include:
Antibiotics: Antibiotic therapy is the mainstay of treatment for bacterial pneumonia. The choice of antibiotics depends on the suspected or confirmed causative organism, local resistance patterns, and individual factors such as age and comorbidities. Commonly prescribed antibiotics for pneumonia include macrolides (such as azithromycin), fluoroquinolones (such as levofloxacin), cephalosporins (such as ceftriaxone), or penicillins (such as amoxicillin-clavulanate).
Antiviral Medications: Antiviral medications may be prescribed for viral pneumonia caused by influenza viruses or other respiratory viruses. Antiviral drugs such as oseltamivir (Tamiflu) may help reduce the severity and duration of symptoms if started early in the course of illness.
Antifungal Therapy: Antifungal medications such as fluconazole or voriconazole may be used to treat fungal pneumonia caused by organisms such as Pneumocystis jirovecii or Histoplasma capsulatum.
Supportive Care: Supportive measures such as rest, hydration, and symptom management (e.g., antipyretics for fever, cough suppressants, or bronchodilators for respiratory symptoms) may help alleviate symptoms and promote recovery.
Oxygen Therapy: Supplemental oxygen therapy may be administered to individuals with severe pneumonia or respiratory distress to maintain adequate oxygenation and improve breathing.
Hospitalization: Hospitalization may be necessary for individuals with severe pneumonia, complications such as respiratory failure or sepsis, or risk factors such as advanced age, immunocompromised status, or comorbid medical conditions. In the hospital setting, intravenous antibiotics, respiratory support, and close monitoring may be provided.