Your cart is currently empty!
Hemorrhoids/Piles
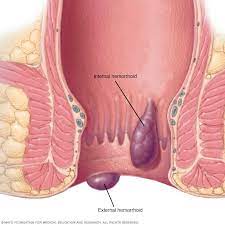
Hemorrhoids, also known as piles, are swollen and inflamed veins in the rectum and anus that can cause discomfort, pain, itching, and bleeding. They are a common condition and can occur internally inside the rectum or externally around the anus. Hemorrhoids can vary in size and severity, ranging from small, mildly irritating swellings to larger, more painful lumps.
Types of Hemorrhoids:
Internal Hemorrhoids: Internal hemorrhoids develop inside the rectum and are usually painless unless they prolapse (protrude) outside the anus during bowel movements. Internal hemorrhoids may cause symptoms such as bleeding, itching, or discomfort.
External Hemorrhoids: External hemorrhoids develop outside the anus beneath the skin and are often more painful than internal hemorrhoids. They may cause symptoms such as pain, swelling, itching, or irritation, particularly during bowel movements or while sitting.
Causes and Risk Factors of Hemorrhoids:
Straining During Bowel Movements: Hemorrhoids are commonly caused by increased pressure on the veins in the rectum and anus, often due to straining during bowel movements. Straining can occur as a result of constipation, diarrhea, or prolonged sitting on the toilet.
Chronic Constipation or Diarrhea: Chronic constipation or diarrhea can contribute to the development of hemorrhoids by increasing pressure on the rectal veins and causing straining during bowel movements.
Pregnancy: Pregnancy can increase the risk of developing hemorrhoids due to hormonal changes, increased pressure on the pelvic veins, and straining during childbirth. Hemorrhoids associated with pregnancy often improve after delivery.
Obesity: Obesity or excess body weight can increase intra-abdominal pressure and contribute to the development of hemorrhoids, particularly if accompanied by a sedentary lifestyle and poor dietary habits.
Low-Fiber Diet: A low-fiber diet lacking in fruits, vegetables, and whole grains can lead to constipation and hard stools, increasing the risk of straining during bowel movements and the development of hemorrhoids.
Sedentary Lifestyle: Prolonged sitting or standing for extended periods, particularly in occupations that require sitting for long hours, can impair blood circulation in the rectal area and contribute to the development of hemorrhoids.
Heavy Lifting: Heavy lifting or strenuous physical activity that involves straining or bearing down can increase intra-abdominal pressure and exacerbate existing hemorrhoids or predispose to their development.
Age: Hemorrhoids become more common with age, with prevalence peaking in adults aged 45-65 years. Age-related changes in connective tissue, weakening of the rectal support structures, and increased incidence of chronic conditions such as constipation may contribute to the development of hemorrhoids.
Symptoms of Hemorrhoids:
The symptoms of hemorrhoids can vary depending on the type, size, and severity of the hemorrhoids. Common symptoms may include:
Rectal Bleeding: Bright red blood on toilet paper, in the toilet bowl, or on stool surfaces after bowel movements is a common symptom of hemorrhoids. The bleeding is typically painless and may occur intermittently.
Anal Itching: Itching or irritation around the anus, often accompanied by a sensation of burning or discomfort, may occur due to exposure to moisture, fecal matter, or irritants in the anal area.
Pain or Discomfort: Pain or discomfort may occur with external hemorrhoids, particularly during bowel movements or while sitting for prolonged periods. Pain may range from mild to severe and may be exacerbated by straining, sitting, or friction.
Swelling or Lump: Swelling, bulging, or protrusion around the anus, particularly during or after bowel movements, may indicate the presence of external hemorrhoids. Internal hemorrhoids may prolapse (protrude) outside the anus and may be felt as a soft, bulging lump.
Anal Leakage: Leakage of mucus or fecal matter from the anus, particularly in cases of prolapsed internal hemorrhoids, may occur due to impaired rectal sphincter function or irritation of the anal mucosa.
Incomplete Evacuation: Difficulty or discomfort with bowel movements, a feeling of incomplete evacuation, or a sensation of rectal fullness may occur due to the presence of internal hemorrhoids or associated symptoms such as rectal bleeding or swelling.
Diagnosis and Treatment of Hemorrhoids:
Diagnosis of hemorrhoids is typically based on a combination of medical history, physical examination, and evaluation of symptoms. Diagnostic tests such as anoscopy, sigmoidoscopy, or colonoscopy may be performed to visualize the rectum and anus and assess for other potential causes of rectal bleeding or anal symptoms.
Treatment of hemorrhoids aims to alleviate symptoms, reduce swelling and inflammation, and improve bowel habits. Treatment options may include:
Lifestyle Modifications:
- Dietary Fiber: Increasing dietary fiber intake through fruits, vegetables, whole grains, and fiber supplements can help soften stools, promote regular bowel movements, and reduce the risk of constipation and straining.
- Hydration: Adequate hydration with water or other non-caffeinated fluids can help soften stools and prevent dehydration, facilitating bowel movements and reducing the risk of constipation.
- Regular Exercise: Engaging in regular physical activity such as walking, swimming, or cycling can help improve bowel function, promote circulation, and reduce the risk of constipation and hemorrhoid formation.
- Avoid Straining: Avoiding straining during bowel movements, minimizing time spent on the toilet, and responding promptly to the urge to defecate can help prevent exacerbation of hemorrhoids and reduce the risk of complications.
Topical Treatments:
- Over-the-Counter (OTC) Products: OTC topical treatments such as hemorrhoid creams, ointments, or suppositories containing ingredients such as hydrocortisone, witch hazel, or phenylephrine may help relieve itching, swelling, or discomfort associated with hemorrhoids.
- Warm Sitz Baths: Soaking the anal area in warm water (sitz baths) for 10-15 minutes several times a day can help soothe irritation, reduce swelling, and promote healing of hemorrhoids.
Medications:
- Topical Anesthetics: Topical anesthetic agents such as lidocaine or benzocaine may be used to provide temporary relief of pain or discomfort associated with hemorrhoids, particularly external hemorrhoids.
- Topical Corticosteroids: Topical corticosteroid medications such as hydrocortisone cream or ointment may be prescribed for short-term use to reduce inflammation and itching associated with hemorrhoids.
Minimally Invasive Procedures:
- Rubber Band Ligation: Rubber band ligation is a common outpatient procedure used to treat symptomatic internal hemorrhoids by placing a small rubber band at the base of the hemorrhoid, cutting off its blood supply, and causing it to shrink and fall off within a few days.
- Sclerotherapy: Sclerotherapy involves injecting a chemical solution into the hemorrhoid to shrink and scar the tissue, reducing blood flow and causing the hemorrhoid to shrink over time.
- Infrared Coagulation: Infrared coagulation (IRC) uses heat energy to cauterize the blood vessels supplying the hemorrhoid, leading to coagulation and shrinkage of the hemorrhoidal tissue.
- Hemorrhoidectomy: Hemorrhoidectomy is a surgical procedure performed under anesthesia to remove large or symptomatic internal or external hemorrhoids that do not respond to conservative treatment measures. Hemorrhoidectomy may be performed using traditional open surgery or minimally invasive techniques such as stapled hemorrhoidopexy (PPH) or transanal hemorrhoidal dearterialization (THD).
Hemorrhoid Banding: Rubber band ligation is a common outpatient procedure used to treat symptomatic internal hemorrhoids by placing a small rubber band at the base of the hemorrhoid, cutting off its blood supply, and causing it to shrink and fall off within a few days.
Injection Therapy: Sclerotherapy involves injecting a chemical solution into the hemorrhoid to shrink and scar the tissue, reducing blood flow and causing the hemorrhoid to shrink over time.
Infrared Coagulation: Infrared coagulation (IRC) uses heat energy to cauterize the blood vessels supplying the hemorrhoid, leading to coagulation and shrinkage of the hemorrhoidal tissue.
Surgical Hemorrhoidectomy: Hemorrhoidectomy is a surgical procedure performed under anesthesia to remove large or symptomatic internal or external hemorrhoids that do not respond to conservative treatment measures. Hemorrhoidectomy may be performed using traditional open surgery or minimally invasive techniques such as stapled hemorrhoidopexy (PPH) or transanal hemorrhoidal dearterialization (THD).