Your cart is currently empty!
Fatty Liver
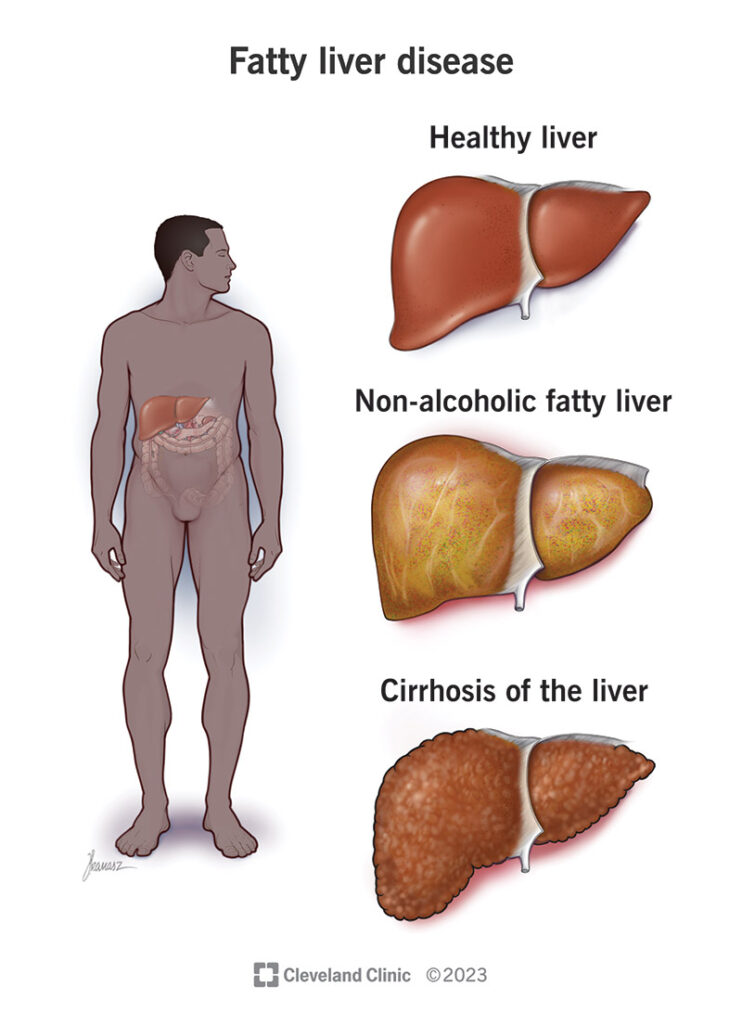
Fatty liver, also known as hepatic steatosis, is a condition characterized by the accumulation of fat within the liver cells (hepatocytes). It is a common liver disorder and can occur due to various factors, including excessive alcohol consumption (alcoholic fatty liver disease) or factors unrelated to alcohol intake (nonalcoholic fatty liver disease, or NAFLD). NAFLD is further categorized into nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH), with NASH being a more severe form associated with inflammation and liver damage.
Causes of Fatty Liver:
-
Alcohol Consumption: Excessive alcohol consumption is a common cause of alcoholic fatty liver disease, leading to the accumulation of fat in the liver cells. Chronic alcohol abuse can result in inflammation, liver injury, and progression to more severe liver diseases such as alcoholic hepatitis or cirrhosis.
-
Obesity and Metabolic Syndrome: Obesity, insulin resistance, type 2 diabetes, dyslipidemia (abnormal lipid levels), and metabolic syndrome are significant risk factors for the development of nonalcoholic fatty liver disease (NAFLD). Insulin resistance and excess adipose tissue contribute to increased fatty acid uptake by the liver, impaired fat metabolism, and accumulation of fat within hepatocytes.
-
Dietary Factors: Consumption of a high-fat, high-calorie diet, particularly one rich in saturated fats, trans fats, and refined carbohydrates, can contribute to the development of fatty liver by promoting weight gain, insulin resistance, and dyslipidemia.
-
Genetic Factors: Genetic factors may predispose some individuals to develop fatty liver disease, particularly nonalcoholic fatty liver disease (NAFLD). Certain genetic variants related to lipid metabolism, insulin sensitivity, and liver function may increase the risk of fatty liver in susceptible individuals.
-
Medications and Toxins: Certain medications, toxins, or environmental exposures may contribute to the development or exacerbation of fatty liver disease. These may include medications such as corticosteroids, methotrexate, tamoxifen, or antiretroviral drugs, as well as exposure to environmental toxins, industrial chemicals, or pollutants.
-
Other Medical Conditions: Other medical conditions such as viral hepatitis (hepatitis C), autoimmune liver diseases, celiac disease, Wilson’s disease, or disorders of lipid metabolism may be associated with an increased risk of fatty liver disease.
Symptoms of Fatty Liver:
Fatty liver disease is often asymptomatic in its early stages and may be diagnosed incidentally during routine medical evaluations or imaging studies. However, as the disease progresses, individuals with fatty liver disease, particularly nonalcoholic steatohepatitis (NASH), may experience symptoms such as:
-
Fatigue: Persistent fatigue or weakness may occur, often due to liver inflammation, impaired liver function, or systemic effects of metabolic dysfunction associated with fatty liver disease.
-
Abdominal Discomfort: Discomfort or pain in the upper right abdomen, near the location of the liver, may occur in some individuals with fatty liver disease, particularly if inflammation or enlargement of the liver is present.
-
Weight Loss: Unintentional weight loss may occur in individuals with advanced fatty liver disease, particularly nonalcoholic steatohepatitis (NASH), due to metabolic dysfunction, loss of appetite, or systemic effects of liver inflammation.
-
Enlarged Liver: Enlargement of the liver (hepatomegaly) may be detected on physical examination or imaging studies in individuals with fatty liver disease, particularly if inflammation, fibrosis, or other complications are present.
-
Jaundice: Jaundice, a yellowing of the skin and eyes, may occur in individuals with advanced liver disease or cirrhosis due to impaired liver function and accumulation of bilirubin in the bloodstream.
-
Ascites: Ascites, the accumulation of fluid in the abdominal cavity, may occur in individuals with advanced liver disease or cirrhosis due to impaired liver function, portal hypertension, and fluid retention.
-
Easy Bruising or Bleeding: Easy bruising, bleeding gums, or frequent nosebleeds may occur in individuals with advanced liver disease or cirrhosis due to impaired liver function and decreased production of clotting factors.
Diagnosis and Treatment of Fatty Liver:
Diagnosis of fatty liver disease is typically based on a combination of medical history, physical examination, laboratory tests, imaging studies (e.g., ultrasound, CT scan, MRI), and liver biopsy (in select cases) to evaluate the extent of liver damage and rule out other liver diseases.
Treatment of fatty liver disease aims to address underlying risk factors, promote liver health, and prevent progression to more severe liver diseases such as cirrhosis or liver failure. Treatment options may include:
-
Lifestyle Modifications:
- Weight Loss: Achieving and maintaining a healthy body weight through diet and regular exercise is a cornerstone of fatty liver disease management, particularly in individuals who are overweight or obese.
- Healthy Diet: Adopting a balanced, nutritious diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help improve metabolic health, reduce inflammation, and promote liver health.
- Physical Activity: Engaging in regular physical activity such as aerobic exercise, strength training, or yoga can help improve insulin sensitivity, promote weight loss, and reduce the risk of fatty liver disease progression.
- Limit Alcohol Intake: For individuals with alcoholic fatty liver disease, limiting or abstaining from alcohol consumption is essential to prevent further liver damage and complications.
-
Medications:
- Insulin Sensitizers: Medications such as metformin or thiazolidinediones (TZDs) may be prescribed to improve insulin sensitivity, reduce liver fat accumulation, and lower the risk of fatty liver disease progression in individuals with insulin resistance or type 2 diabetes.
- Lipid-Lowering Agents: Statin medications or other lipid-lowering agents may be prescribed to help manage dyslipidemia (abnormal lipid levels) and reduce cardiovascular risk in individuals with fatty liver disease.
- Antioxidants: Antioxidant supplements such as vitamin E may be recommended to help reduce liver inflammation and oxidative stress in individuals with nonalcoholic steatohepatitis (NASH), although the evidence for their effectiveness is limited.
-
Management of Comorbid Conditions:
- Diabetes Control: Optimal management of diabetes through lifestyle modifications, medication therapy, and regular monitoring of blood glucose levels is essential to prevent complications and reduce the risk of fatty liver disease progression.
- Hypertension Control: Controlling hypertension (high blood pressure) through lifestyle modifications and medication therapy is important to reduce the risk of cardiovascular complications and liver disease progression in individuals with fatty liver disease.
-
Screening and Treatment of Complications:
- Liver Cancer Screening: Regular surveillance for liver cancer (hepatocellular carcinoma) using imaging studies such as ultrasound, CT scan, or MRI may be recommended for individuals with advanced liver disease or cirrhosis due to fatty liver disease.
- Treatment of Cirrhosis Complications: Management of complications such as ascites, hepatic encephalopathy, variceal bleeding, or hepatorenal syndrome in individuals with cirrhosis due to fatty liver disease may involve medications, dietary modifications, procedures (e.g., paracentesis, transjugular intrahepatic portosystemic shunt), or liver transplantation in select cases.
-
Liver Transplantation: Liver transplantation may be considered for individuals with advanced liver disease, cirrhosis, or liver failure due to fatty liver disease who have failed medical therapy or developed life-threatening complications. Liver transplantation involves surgical replacement of the diseased liver with a healthy liver from a deceased or living donor.