Your cart is currently empty!
Copd
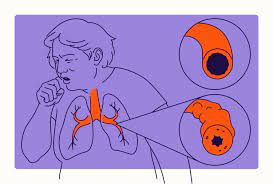
Chronic obstructive pulmonary disease (COPD) is a progressive respiratory condition characterized by persistent airflow limitation and difficulty breathing. COPD encompasses a group of chronic lung disorders, including emphysema and chronic bronchitis, which commonly coexist and share similar symptoms and risk factors. COPD is a leading cause of morbidity and mortality worldwide and is primarily associated with long-term exposure to harmful inhalants, such as cigarette smoke, air pollution, or occupational dust and chemicals.
Causes and Risk Factors of COPD:
Tobacco Smoke: Cigarette smoking is the most significant risk factor for COPD, accounting for the majority of cases. Long-term exposure to tobacco smoke leads to chronic inflammation, airway damage, and progressive narrowing of the airways, contributing to the development and progression of COPD.
Environmental Exposures: Long-term exposure to indoor and outdoor air pollutants, such as biomass fuel smoke, industrial pollutants, or vehicle emissions, can increase the risk of COPD. Occupational exposures to dust, fumes, or chemicals in certain industries (e.g., mining, construction, agriculture) may also predispose to COPD.
Genetic Factors: Genetic predisposition may play a role in COPD susceptibility, particularly in individuals with alpha-1 antitrypsin deficiency (AATD), a hereditary condition that affects lung function and increases the risk of emphysema, particularly in nonsmokers or individuals with minimal smoking history.
Age and Gender: COPD is more common in older adults, particularly those over the age of 40-50 years. Men have historically been more affected by COPD than women, although the gender gap has narrowed in recent years due to increased smoking prevalence among women.
Respiratory Infections: Recurrent respiratory infections, such as viral infections (e.g., influenza, respiratory syncytial virus) or bacterial infections (e.g., pneumonia), can exacerbate COPD symptoms and accelerate disease progression, particularly in susceptible individuals.
Indoor Air Quality: Indoor exposure to biomass fuels (e.g., wood, coal, animal dung) used for cooking or heating in poorly ventilated settings, particularly in low- and middle-income countries, can contribute to the development of COPD.
Symptoms of COPD:
The symptoms of COPD can vary in severity and may include:
Chronic Cough: Persistent cough that produces sputum (mucus) and may be worse in the morning or with exposure to irritants.
Shortness of Breath: Dyspnea (shortness of breath) that worsens with physical activity (exertional dyspnea) and may progress to occur at rest as the disease advances.
Wheezing: Wheezing or whistling sounds when breathing, particularly during exhalation, due to airflow obstruction in the airways.
Chest Tightness: Feelings of tightness, discomfort, or pressure in the chest, which may be exacerbated by respiratory infections or environmental triggers.
Chronic Mucus Production: Chronic production of sputum (mucus) from the lungs, which may be clear, white, yellow, green, or blood-tinged in color.
Fatigue: Generalized fatigue, weakness, or reduced stamina, particularly during periods of increased respiratory symptoms or exacerbations.
Weight Loss: Unintentional weight loss or muscle wasting, which may occur as a result of increased energy expenditure due to breathing difficulties or systemic inflammation.
Cyanosis: Cyanosis (bluish discoloration) of the lips, fingertips, or nail beds, particularly in advanced stages of COPD due to hypoxemia (low oxygen levels) in the blood.
Diagnosis and Treatment of COPD:
Diagnosis of COPD is based on a combination of medical history, physical examination, pulmonary function tests, and imaging studies. Diagnostic tests may include:
Pulmonary Function Tests (PFTs): Spirometry is the primary test used to assess lung function and diagnose airflow obstruction characteristic of COPD. Other tests such as lung volume measurements or diffusing capacity may also be performed to evaluate lung function and severity of disease.
Chest X-ray or CT Scan: Imaging studies such as chest X-ray or CT scan may be ordered to assess for signs of lung hyperinflation, emphysema, or other structural abnormalities.
Treatment of COPD aims to alleviate symptoms, improve lung function, prevent disease progression, and reduce the risk of exacerbations. Treatment options may include:
Smoking Cessation: The most important intervention for COPD management is smoking cessation. Quitting smoking can help slow disease progression, improve lung function, and reduce respiratory symptoms and exacerbations.
Medications:
- Bronchodilators: Bronchodilator medications such as short-acting beta-agonists (SABAs), long-acting beta-agonists (LABAs), or anticholinergic agents (LAMAs) can help relax and widen the airways, improving airflow and relieving symptoms of COPD.
- Inhaled Corticosteroids: Inhaled corticosteroid medications may be prescribed as adjunctive therapy for individuals with moderate to severe COPD and frequent exacerbations, particularly in combination with long-acting bronchodilators (LABA/LAMA combination therapy).
- Phosphodiesterase-4 (PDE-4) Inhibitors: Oral PDE-4 inhibitors such as roflumilast may be used as add-on therapy for individuals with severe COPD and chronic bronchitis who have frequent exacerbations despite optimal bronchodilator therapy.
Pulmonary Rehabilitation: Pulmonary rehabilitation programs incorporating exercise training, education, nutritional counseling, and psychosocial support can help improve exercise capacity, reduce dyspnea, and enhance quality of life in individuals with COPD.
Oxygen Therapy: Long-term oxygen therapy (LTOT) may be prescribed for individuals with severe COPD and chronic hypoxemia to improve oxygenation, relieve symptoms, and reduce the risk of complications such as pulmonary hypertension or cor pulmonale.
Vaccinations: Annual influenza vaccination and pneumococcal vaccination are recommended for individuals with COPD to reduce the risk of respiratory infections and exacerbations.
Surgical Interventions: Surgical options such as lung volume reduction surgery (LVRS) or lung transplantation may be considered for selected individuals with severe COPD who have significant symptoms and impaired quality of life despite optimal medical therapy.
Management of Exacerbations: Prompt recognition and management of COPD exacerbations, which may involve bronchodilator therapy, systemic corticosteroids, antibiotics (if bacterial infection is suspected), and supportive care, can help minimize disease-related complications and hospitalizations.