Your cart is currently empty!
Cervical Spondylitis
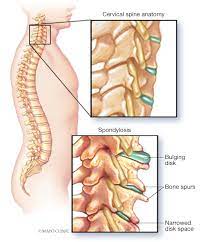
Cervical spondylitis, also known as cervical spondylosis or cervical osteoarthritis, is a degenerative condition affecting the cervical spine, which is the portion of the vertebral column located in the neck region. Cervical spondylitis is characterized by wear and tear of the cervical spine joints, intervertebral discs, and surrounding structures, leading to various symptoms and functional limitations.
Causes of Cervical Spondylitis:
Cervical spondylitis typically develops over time as a result of age-related changes in the spine, although certain factors may increase the risk of developing the condition, including:
Age: The risk of cervical spondylitis increases with age, as the spine undergoes degenerative changes over time.
Degenerative Changes: Wear and tear of the cervical spine joints, intervertebral discs, and ligaments due to repetitive stress, poor posture, or mechanical factors contribute to the development of cervical spondylitis.
Genetic Factors: Genetic predisposition may play a role in the development of cervical spondylitis, as some individuals may inherit traits that increase their susceptibility to spinal degeneration.
Smoking: Tobacco smoking has been associated with an increased risk of developing cervical spondylitis, as it may accelerate the degenerative changes in the spine.
Occupational Factors: Jobs or activities that involve repetitive neck movements, heavy lifting, or prolonged sitting or standing may increase the risk of developing cervical spondylitis.
Symptoms of Cervical Spondylitis:
The symptoms of cervical spondylitis can vary depending on the severity of degeneration, the presence of nerve compression, and individual factors. Common symptoms may include:
Neck Pain: Chronic or intermittent neck pain, stiffness, or discomfort, particularly with movement or prolonged sitting or standing.
Radiating Pain: Pain that radiates from the neck into the shoulders, arms, hands, or fingers, often following the path of the affected nerve roots.
Numbness or Tingling: Numbness, tingling, or pins-and-needles sensations in the arms, hands, or fingers, which may indicate nerve compression.
Weakness: Weakness or difficulty gripping objects, lifting the arms, or performing fine motor tasks due to nerve compression or muscle weakness.
Headaches: Cervicogenic headaches, which originate from the cervical spine, may occur as a result of cervical spondylitis.
Loss of Range of Motion: Decreased flexibility or range of motion in the neck, making it difficult to turn the head or perform daily activities.
Muscle Spasms: Muscle tightness or spasms in the neck, shoulders, or upper back, which may exacerbate symptoms.
Diagnosis and Treatment of Cervical Spondylitis:
Diagnosis of cervical spondylitis typically involves a combination of medical history, physical examination, and diagnostic tests such as:
Imaging Studies: X-rays, MRI, or CT scans may be ordered to visualize the cervical spine and identify any degenerative changes, such as bone spurs, disc herniations, or narrowing of the spinal canal.
Electrodiagnostic Tests: Electromyography (EMG) or nerve conduction studies may be performed to assess the function of the nerves and muscles in the arms and hands and determine the extent of nerve compression or damage.
Treatment of cervical spondylitis aims to relieve symptoms, improve function, and prevent complications. Conservative treatment options may include:
Pain Medications: Over-the-counter or prescription medications such as NSAIDs (nonsteroidal anti-inflammatory drugs), muscle relaxants, or neuropathic pain medications may be prescribed to alleviate pain and inflammation.
Physical Therapy: Physical therapy exercises, stretches, and modalities such as heat or ice therapy may help relieve pain, improve flexibility, and strengthen the muscles supporting the cervical spine.
Cervical Traction: Cervical traction therapy may be used to gently stretch the cervical spine and relieve pressure on compressed nerves or discs.
Epidural Steroid Injections: Corticosteroid injections into the epidural space around the cervical nerves may be recommended to reduce inflammation and provide temporary pain relief.
Chiropractic Manipulation: Spinal manipulation performed by a qualified chiropractor may help alleviate symptoms of cervical spondylitis by improving spinal alignment and reducing nerve compression.
Acupuncture: Acupuncture, a traditional Chinese medicine technique involving the insertion of thin needles into specific points on the body, may help relieve pain and improve symptoms of cervical spondylitis for some individuals.
Lifestyle Modifications: Adopting healthy lifestyle habits such as maintaining good posture, avoiding prolonged sitting or standing, using proper ergonomics, and engaging in regular exercise can help prevent or manage cervical spondylitis.
Surgery may be considered in severe or refractory cases of cervical spondylitis that do not respond to conservative treatments. Surgical interventions such as discectomy, laminectomy, cervical fusion, or artificial disc replacement may be performed to decompress the affected nerves, stabilize the spine, or address structural abnormalities.