Your cart is currently empty!
Bronchitis
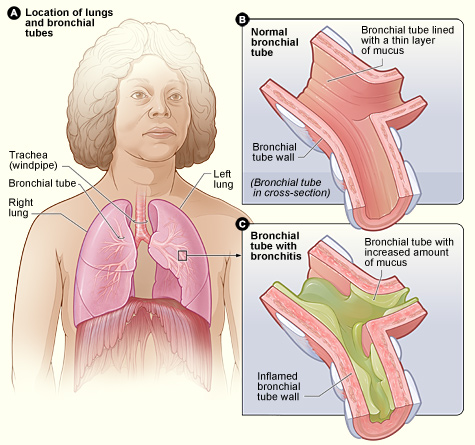
Bronchitis is an inflammation of the bronchial tubes, the air passages that carry air to the lungs. It can be acute or chronic and is commonly caused by viral infections, although bacterial infections, environmental factors, and other irritants can also contribute to its development.
Types of Bronchitis:
Acute Bronchitis: Acute bronchitis is a temporary inflammation of the bronchial tubes, often resulting from viral infections such as the common cold or influenza. It usually resolves on its own within a few weeks, although cough may persist for several weeks after other symptoms have resolved.
Chronic Bronchitis: Chronic bronchitis is a long-term inflammation of the bronchial tubes, characterized by persistent cough with sputum production for at least three months in two consecutive years. It is a type of chronic obstructive pulmonary disease (COPD) and is commonly associated with smoking or long-term exposure to irritants such as air pollution or occupational dust and chemicals.
Causes of Bronchitis:
Viral Infections: Acute bronchitis is often caused by viral infections such as rhinovirus, influenza virus, respiratory syncytial virus (RSV), or adenovirus. Viral bronchitis is highly contagious and commonly spreads through respiratory droplets from coughing or sneezing.
Bacterial Infections: Bacterial infections such as Mycoplasma pneumoniae or Bordetella pertussis (whooping cough) can also cause acute bronchitis, particularly in individuals with weakened immune systems or underlying respiratory conditions.
Environmental Irritants: Exposure to environmental irritants such as cigarette smoke, air pollution, dust, or chemical fumes can irritate the bronchial tubes and trigger inflammation, leading to acute or chronic bronchitis.
Allergies: Allergic reactions to airborne allergens such as pollen, mold, or animal dander may exacerbate symptoms of bronchitis, particularly in individuals with allergic rhinitis or asthma.
Symptoms of Bronchitis:
The symptoms of bronchitis can vary depending on the underlying cause, duration, and severity of the condition. Common symptoms may include:
Cough: Persistent cough that may produce clear, white, yellow, or greenish sputum (mucus). Cough may be dry initially and later become productive as inflammation increases.
Shortness of Breath: Dyspnea (shortness of breath) or wheezing, particularly with exertion or during coughing spells. Breathing difficulties may be more pronounced in individuals with underlying respiratory conditions such as asthma or COPD.
Chest Discomfort: Chest discomfort, tightness, or pain, which may worsen with coughing or deep breathing due to inflammation of the bronchial tubes.
Fatigue: Generalized fatigue, malaise, or feeling unwell, particularly during acute illness or exacerbations of bronchitis.
Sore Throat: Sore or scratchy throat, particularly in cases of viral bronchitis accompanied by upper respiratory symptoms such as nasal congestion or postnasal drip.
Fever: Low-grade fever (less than 100.4°F or 38°C) may occur in cases of acute bronchitis, particularly if associated with viral respiratory infections.
Diagnosis and Treatment of Bronchitis:
Diagnosis of bronchitis is based on a combination of medical history, physical examination, and diagnostic tests. Diagnostic tests may include:
Medical History: A healthcare provider will review the patient’s medical history, including symptoms, duration of illness, recent respiratory infections, exposure to irritants, smoking history, and underlying medical conditions.
Physical Examination: A physical examination may be performed to assess respiratory symptoms, listen to lung sounds (auscultation), and evaluate for signs of inflammation or infection.
Diagnostic Tests: Diagnostic tests such as chest X-ray, sputum culture, or pulmonary function tests may be ordered to rule out other respiratory conditions and assess lung function.
Treatment of bronchitis aims to alleviate symptoms, reduce inflammation, and prevent complications. Treatment options may include:
Symptomatic Relief: Over-the-counter medications such as cough suppressants, expectorants, or pain relievers (e.g., acetaminophen or ibuprofen) may help relieve symptoms such as cough, chest discomfort, or fever.
Hydration: Adequate hydration with water, herbal teas, or clear fluids can help loosen mucus and soothe irritated airways, promoting expectoration and symptom relief.
Bronchodilators: Inhalation of bronchodilator medications such as short-acting beta-agonists (SABAs) or anticholinergic agents (LAMAs) may help relax and widen the airways, improving airflow and relieving symptoms of bronchitis, particularly in individuals with underlying airway obstruction or asthma.
Rest and Recovery: Rest, adequate sleep, and avoidance of strenuous activities can help conserve energy, support immune function, and promote recovery from acute bronchitis.
Smoking Cessation: Smoking cessation is essential for individuals with bronchitis, particularly those with chronic bronchitis or COPD, as continued smoking can worsen symptoms, accelerate disease progression, and increase the risk of complications.
Avoidance of Irritants: Minimizing exposure to environmental irritants such as cigarette smoke, air pollution, dust, or chemical fumes can help prevent exacerbations and reduce the risk of recurrent bronchitis.
Antibiotics: Antibiotic therapy is not routinely recommended for acute bronchitis caused by viral infections, as antibiotics are ineffective against viruses and may contribute to antibiotic resistance. However, antibiotics may be prescribed for bacterial bronchitis or secondary bacterial infections complicating acute illness.
Inhaled Corticosteroids: Inhaled corticosteroid medications may be prescribed for individuals with chronic bronchitis or COPD, particularly in combination with long-acting bronchodilators, to reduce airway inflammation and prevent exacerbations.