Your cart is currently empty!
Asthma
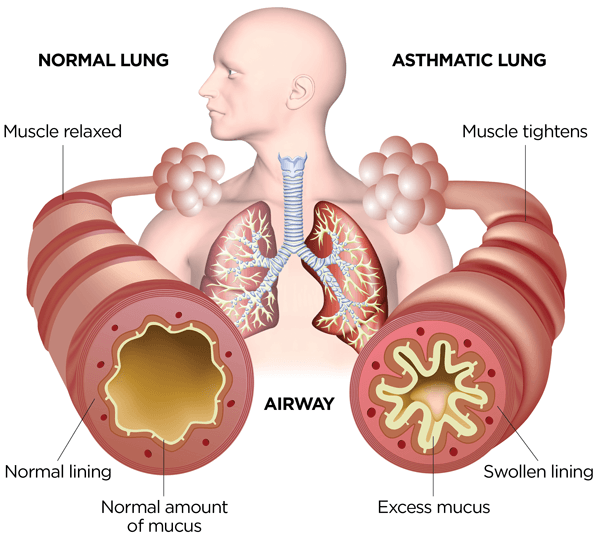
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to recurrent episodes of wheezing, coughing, chest tightness, and shortness of breath. It is a common condition that affects people of all ages, and its severity can range from mild to severe, with symptoms varying in frequency and intensity over time.
Causes and Triggers of Asthma:
Genetic Factors: Asthma tends to run in families, suggesting a genetic predisposition to the condition. Individuals with a family history of asthma or allergic conditions are at increased risk of developing asthma themselves.
Environmental Factors: Exposure to certain environmental triggers can exacerbate asthma symptoms or precipitate asthma attacks. Common triggers include airborne allergens such as pollen, dust mites, mold, pet dander, or cockroach allergens; respiratory irritants such as cigarette smoke, air pollution, or strong odors; viral respiratory infections such as the common cold or influenza; physical exertion or exercise; cold air or changes in weather; and occupational exposures to dust, chemicals, or fumes.
Allergic Sensitization: Allergic asthma is characterized by immune-mediated inflammation of the airways triggered by exposure to allergens such as pollen, mold, dust mites, animal dander, or certain foods. Sensitization to allergens can lead to the production of immunoglobulin E (IgE) antibodies and activation of mast cells, eosinophils, and other inflammatory cells, contributing to airway inflammation and bronchoconstriction.
Non-Allergic Triggers: Non-allergic asthma may be triggered by non-immune mechanisms such as respiratory infections, cold air, exercise, stress, or exposure to irritants or pollutants. These triggers can induce airway inflammation and bronchospasm in susceptible individuals, leading to asthma symptoms.
Risk Factors: Several risk factors may increase the likelihood of developing asthma, including a family history of asthma or allergic conditions, history of respiratory infections or allergies in childhood, exposure to tobacco smoke or indoor air pollutants, obesity, low socioeconomic status, and certain occupational exposures.
Symptoms of Asthma:
The symptoms of asthma can vary in severity and frequency and may include:
Wheezing: Wheezing is a high-pitched whistling sound heard during breathing, particularly during exhalation, due to narrowing of the airways and airflow obstruction.
Cough: Coughing is a common symptom of asthma and may be dry or productive, particularly during asthma exacerbations or in response to triggers such as cold air, exercise, or allergen exposure.
Shortness of Breath: Dyspnea (shortness of breath) or difficulty breathing, particularly with exertion, may occur during asthma attacks or exacerbations.
Chest Tightness: Chest tightness or discomfort, often described as a feeling of pressure or constriction in the chest, may accompany asthma symptoms, particularly during exacerbations.
Increased Respiratory Rate: Rapid or shallow breathing (tachypnea) may occur during asthma exacerbations as the body attempts to compensate for airflow obstruction and maintain adequate oxygenation.
Cyanosis: Cyanosis (bluish discoloration) of the lips, fingertips, or nail beds may occur in severe cases of asthma due to hypoxemia (low oxygen levels) in the blood.
Cough Variant Asthma: Some individuals with asthma may present primarily with chronic cough as the predominant symptom, particularly in the absence of wheezing or dyspnea.
Diagnosis and Treatment of Asthma:
Diagnosis of asthma is based on a combination of medical history, physical examination, lung function tests, and assessment of symptoms and triggers. Diagnostic tests may include:
Spirometry: Spirometry is the primary test used to assess lung function and diagnose airflow obstruction characteristic of asthma. Spirometry measures parameters such as forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) and can help determine the presence and severity of airflow limitation.
Peak Expiratory Flow (PEF) Monitoring: Peak flow meters are portable devices used to measure peak expiratory flow rate, which reflects the maximal airflow generated during forced expiration. PEF monitoring can help assess airflow variability and monitor asthma control over time.
Bronchoprovocation Testing: Bronchoprovocation tests such as methacholine challenge or exercise challenge may be performed to assess airway hyperresponsiveness and confirm the diagnosis of asthma in individuals with inconclusive spirometry results.
Treatment of asthma aims to achieve and maintain asthma control, reduce symptoms and exacerbations, and minimize the risk of complications. Treatment options may include:
Medications:
- Inhaled Corticosteroids (ICS): Inhaled corticosteroid medications such as fluticasone, budesonide, or beclomethasone are the cornerstone of asthma therapy and help reduce airway inflammation, prevent asthma symptoms, and improve lung function when used regularly as prescribed.
- Long-Acting Beta-Agonists (LABAs): Long-acting beta-agonist medications such as salmeterol or formoterol may be used in combination with ICS as controller therapy to provide bronchodilation and improve asthma control.
- Short-Acting Beta-Agonists (SABAs): Short-acting beta-agonist medications such as albuterol or levalbuterol are used as rescue or reliever medications to provide rapid relief of asthma symptoms and bronchospasm during acute exacerbations or as needed for symptom relief.
- Leukotriene Receptor Antagonists (LTRAs): Leukotriene receptor antagonist medications such as montelukast or zafirlukast may be used as add-on therapy for individuals with asthma, particularly in cases of allergic asthma or exercise-induced bronchoconstriction.
- Biologic Therapies: Biologic therapies such as monoclonal antibodies targeting specific inflammatory pathways (e.g., anti-IgE therapy with omalizumab, anti-IL-5 therapy with mepolizumab or reslizumab) may be considered for individuals with severe asthma and eosinophilic inflammation who do not respond adequately to conventional therapy.
- Oral Corticosteroids: Oral corticosteroid medications such as prednisone or methylprednisolone may be prescribed for short-term use during asthma exacerbations or as adjunctive therapy for individuals with severe asthma uncontrolled with other medications.
Rescue Medications: Short-acting beta-agonist (SABA) inhalers such as albuterol or levalbuterol are used as rescue or reliever medications to provide rapid relief of asthma symptoms and bronchospasm during acute exacerbations or as needed for symptom relief.
Controller Medications: Long-term controller medications such as inhaled corticosteroids (ICS), long-acting beta-agonists (LABAs), leukotriene receptor antagonists (LTRAs), or biologic therapies are used to prevent asthma symptoms, reduce airway inflammation, and improve lung function when used regularly as prescribed.
Allergy Management: Identification and avoidance of triggers such as airborne allergens (e.g., pollen, dust mites, pet dander) can help minimize asthma symptoms and exacerbations in individuals with allergic asthma. Allergy testing and immunotherapy (allergy shots) may be considered for individuals with specific allergen sensitivities.
Asthma Action Plan: An asthma action plan is a personalized written document developed in collaboration with a healthcare provider that outlines individualized instructions for asthma management, including medication use, symptom monitoring, and steps to take in case of worsening symptoms or asthma exacerbations.
Lifestyle Modifications: Lifestyle modifications such as smoking cessation, avoidance of respiratory irritants or triggers, regular exercise, maintenance of a healthy weight, and adherence to prescribed medications can help improve asthma control and reduce the risk of exacerbations.
Regular Follow-Up: Regular follow-up with a healthcare provider, such as a primary care physician, pulmonologist, or allergist, is essential for monitoring asthma control, adjusting treatment as needed, and providing education and support for individuals with asthma and their caregivers.