Your cart is currently empty!
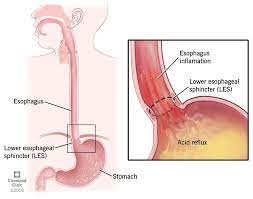
GERD
Gastroesophageal reflux disease (GERD) is a chronic digestive disorder characterized by the reflux of stomach acid and digestive juices into the esophagus, leading to symptoms such as heartburn, regurgitation, and discomfort. GERD occurs when the lower esophageal sphincter (LES), a ring of muscle at the junction of the esophagus and stomach, relaxes abnormally or weakens, allowing stomach contents to flow back up into the esophagus.
Symptoms of GERD: The symptoms of GERD can vary in severity and frequency among individuals, but common symptoms may include:
Heartburn: A burning sensation or discomfort in the chest, often behind the breastbone, that may worsen after eating, lying down, or bending over. Heartburn is one of the hallmark symptoms of GERD and is caused by irritation of the esophageal lining by stomach acid.
Regurgitation: The sensation of acid reflux or sour-tasting fluid moving up into the throat or mouth, often accompanied by a bitter or acidic taste. Regurgitation may occur spontaneously or be triggered by bending over, lying down, or eating large meals.
Dysphagia: Difficulty swallowing or a sensation of food getting stuck in the throat or chest. Dysphagia may occur if inflammation or narrowing of the esophagus (esophageal stricture) develops due to chronic acid reflux.
Chest Pain: Chest pain or discomfort that may mimic symptoms of a heart attack, particularly in individuals with severe or atypical symptoms of GERD. Chest pain associated with GERD is typically non-cardiac in origin and may be relieved by antacids or changes in body position.
Regurgitation of Food or Liquid: The involuntary passage of partially digested food or liquid from the stomach back up into the esophagus or mouth, often occurring shortly after eating or lying down.
Chronic Cough: A persistent cough that is not related to respiratory infections or other underlying lung conditions, but may be triggered or worsened by acid reflux into the throat or airways.
Hoarseness or Sore Throat: Hoarseness, sore throat, or irritation of the throat due to acid reflux or regurgitation of stomach contents into the throat, larynx, or vocal cords.
Laryngopharyngeal Reflux (LPR): LPR occurs when stomach acid refluxes into the throat or voice box (larynx), leading to symptoms such as chronic throat clearing, throat irritation, cough, or voice changes (e.g., hoarseness).
Causes and Risk Factors of GERD: GERD occurs due to dysfunction of the lower esophageal sphincter (LES) and factors that increase intra-abdominal pressure or disrupt the normal balance of digestive processes. Common causes and risk factors for GERD may include:
Weak or Relaxing LES: Dysfunction or weakening of the lower esophageal sphincter (LES), a ring of muscle that normally prevents stomach contents from refluxing into the esophagus, may allow acid reflux to occur more frequently or with greater severity.
Hiatal Hernia: A hiatal hernia occurs when a portion of the stomach protrudes through the diaphragm into the chest cavity, disrupting the normal anatomy and function of the LES and increasing the risk of acid reflux.
Obesity or Excess Weight: Excess body weight, particularly abdominal obesity, can increase intra-abdominal pressure and put pressure on the stomach, leading to acid reflux and GERD symptoms.
Dietary Factors: Certain dietary factors may contribute to GERD symptoms, including consumption of spicy or fatty foods, acidic foods or beverages (e.g., citrus fruits, tomatoes, coffee, alcohol), chocolate, peppermint, or carbonated beverages.
Smoking: Smoking tobacco or exposure to secondhand smoke can weaken the LES, impair esophageal motility, and increase the production of stomach acid, leading to an increased risk of GERD.
Pregnancy: Hormonal changes, increased intra-abdominal pressure, and mechanical factors associated with pregnancy can contribute to the development or exacerbation of GERD symptoms in pregnant women, particularly during the third trimester.
Certain Medications: Some medications may increase the risk of GERD or exacerbate symptoms by relaxing the LES, increasing stomach acid production, or causing irritation of the esophageal lining. These may include nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, certain blood pressure medications (e.g., calcium channel blockers), sedatives, antidepressants, or medications for asthma or allergies.
Delayed Gastric Emptying: Delayed gastric emptying (gastroparesis) or impaired stomach motility can lead to an accumulation of stomach contents and increased gastric pressure, predisposing to acid reflux and GERD symptoms.
Diagnosis of GERD: Diagnosis of GERD is typically based on a combination of clinical evaluation, medical history, symptom assessment, physical examination, and diagnostic tests to evaluate the presence and severity of acid reflux and assess for complications. Diagnostic tests for GERD may include:
Symptom Assessment: Evaluation of typical GERD symptoms such as heartburn, regurgitation, chest pain, or difficulty swallowing, as well as assessment of symptom frequency, severity, duration, and triggers.
Upper Endoscopy (EGD): Upper endoscopy or esophagogastroduodenoscopy (EGD) may be performed to visualize the esophagus, stomach, and upper gastrointestinal tract, assess for signs of inflammation, erosions, ulcers, strictures, or Barrett’s esophagus, and obtain biopsies if needed.
Esophageal pH Monitoring: Esophageal pH monitoring, including ambulatory pH monitoring (pH probe study) or wireless pH monitoring (Bravo capsule), may be used to measure acid reflux episodes, assess esophageal pH levels, and correlate symptoms with acid reflux events over a 24-hour period.
Esophageal Manometry: Esophageal manometry may be performed to evaluate esophageal motility, assess LES function and relaxation, and rule out other esophageal motility disorders or dysmotility syndromes.
Barium Swallow: Barium swallow or upper gastrointestinal series may be used to visualize the esophagus, stomach, and upper digestive tract using X-rays after ingestion of a contrast agent (barium), allowing assessment of anatomical abnormalities, strictures, or hiatal hernia.
Laboratory Tests: Laboratory tests such as complete blood count (CBC), comprehensive metabolic panel (CMP), or fecal occult blood test (FOBT) may be ordered to evaluate for anemia, electrolyte imbalances, or other abnormalities associated with GERD or its complications.
Treatment of GERD: Treatment of GERD aims to alleviate symptoms, reduce the frequency and severity of acid reflux, heal esophageal inflammation or erosions, and prevent complications such as esophagitis, strictures, or Barrett’s esophagus. Treatment options for GERD may include:
Lifestyle Modifications:
- Dietary Changes: Avoiding trigger foods or beverages that exacerbate symptoms, such as spicy foods, fatty foods, acidic foods or drinks, caffeine, alcohol, chocolate, or carbonated beverages.
- Weight Management: Achieving and maintaining a healthy weight through diet, exercise, and lifestyle modifications to reduce intra-abdominal pressure and decrease the risk of acid reflux.
- Elevating the Head of the Bed: Raising the head of the bed by 6 to 8 inches or using wedge-shaped pillows to elevate the upper body during sleep to prevent nighttime reflux and promote gastric emptying.
- Smoking Cessation: Quitting smoking or avoiding exposure to tobacco smoke to reduce the risk of LES relaxation, increase esophageal motility, and improve GERD symptoms.
Medications:
- Antacids: Over-the-counter antacid medications such as calcium carbonate (e.g., Tums), magnesium hydroxide (e.g., Maalox), or aluminum hydroxide (e.g., Mylanta) may be used to neutralize stomach acid and provide rapid relief of heartburn or acid reflux symptoms.
- H2 Receptor Antagonists: Histamine H2 receptor antagonists such as ranitidine (Zantac), famotidine (Pepcid), or cimetidine (Tagamet) may be used to reduce gastric acid secretion and alleviate symptoms of GERD, although they are less effective than proton pump inhibitors (PPIs) for healing esophagitis or preventing complications.
- Proton Pump Inhibitors (PPIs): Proton pump inhibitors such as omeprazole (Prilosec), esomeprazole (Nexium), lansoprazole (Prevacid), pantoprazole (Protonix), or rabeprazole (Aciphex) are the mainstay of treatment for GERD and work by inhibiting gastric acid secretion, promoting healing of esophageal mucosa, and preventing acid-related complications.
- Prokinetic Agents: Prokinetic medications such as metoclopramide (Reglan) or domperidone may be prescribed to enhance gastrointestinal motility, improve esophageal clearance, and reduce acid reflux in individuals with delayed gastric emptying or refractory GERD symptoms.
Surgical Interventions:
- Fundoplication: Laparoscopic fundoplication surgery may be considered in individuals with severe or refractory GERD symptoms who do not respond to medical therapy or lifestyle modifications. Fundoplication involves wrapping the upper part of the stomach (fundus) around the lower esophagus to reinforce the LES and prevent acid reflux.
- LINX Device: The LINX Reflux Management System is a minimally invasive surgical option for GERD that involves placement of a small, flexible magnetic ring around the esophagus to augment the LES and prevent reflux while allowing normal swallowing and belching.
Endoscopic Treatments:
- Endoscopic Procedures: Endoscopic techniques such as endoscopic mucosal resection (EMR), radiofrequency ablation (RFA), cryotherapy, or endoscopic suturing may be used to treat complications of GERD such as Barrett’s esophagus, dysplasia, or early-stage esophageal cancer.
Monitoring and Follow-Up: Regular monitoring and follow-up care with a healthcare provider, such as a gastroenterologist or primary care physician, are important for individuals with GERD to assess treatment response, monitor symptom control, evaluate for complications, and adjust treatment as needed. Long-term management of GERD may involve periodic evaluations, medication adjustments, lifestyle modifications, and ongoing support to optimize outcomes and improve quality of life.
Prognosis: The prognosis of GERD is generally good with appropriate treatment and management, as most individuals experience significant symptom relief and improvement in quality of life with medical therapy, lifestyle modifications, or surgical interventions. However, untreated or poorly controlled GERD can lead to complications such as esophagitis, strictures, Barrett’s esophagus, or esophageal adenocarcinoma over time, highlighting the importance of early diagnosis, prompt treatment, and regular monitoring for individuals with GERD.