Your cart is currently empty!
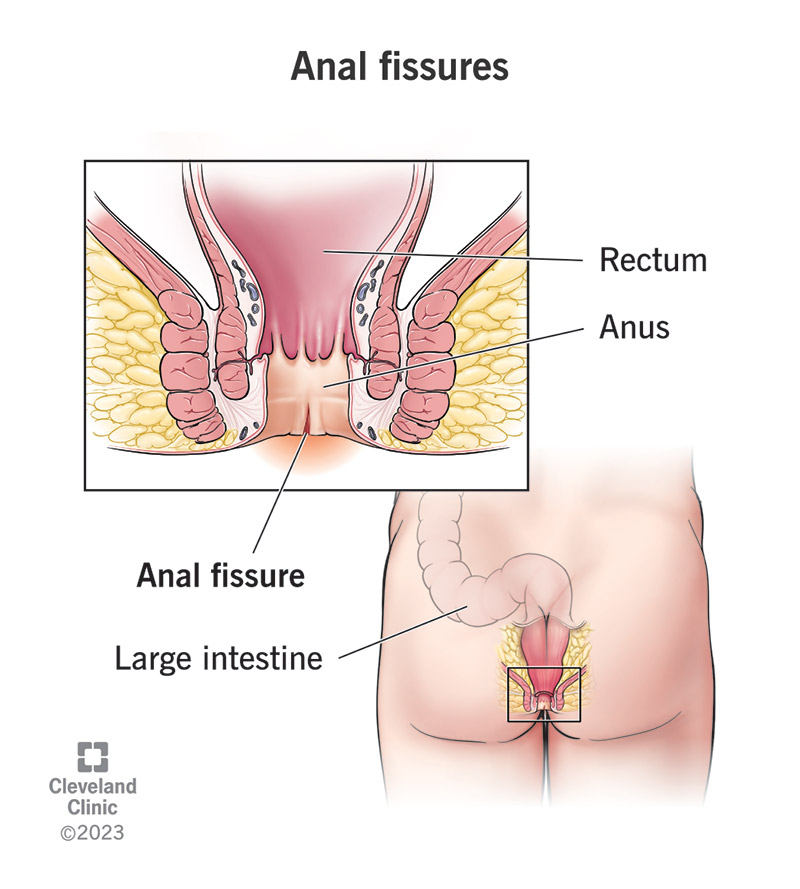
Anal Fissure
An anal fissure is a tear or split in the lining of the anal canal, the passage through which stool passes out of the body. Anal fissures are a common condition and can cause pain, discomfort, and bleeding during bowel movements. They can occur in people of all ages but are more common in infants, young children, and adults between the ages of 20 and 40.
Causes of Anal Fissures:
-
Trauma: The most common cause of anal fissures is trauma or injury to the delicate lining of the anal canal. Trauma may occur due to passing hard or large stools, straining during bowel movements, or repeated irritation from diarrhea.
-
Constipation: Chronic constipation, characterized by infrequent bowel movements and hard stools, can increase the risk of anal fissures by causing straining during bowel movements and stretching or tearing of the anal tissue.
-
Diarrhea: Persistent diarrhea or frequent bowel movements can irritate the anal canal and increase the risk of developing anal fissures, particularly if accompanied by excessive wiping or cleaning of the anal area.
-
Childbirth: Women may develop anal fissures as a result of trauma to the anal canal during childbirth, particularly if they experience tears or lacerations of the perineum (the area between the vagina and anus) or undergo episiotomy (a surgical incision to enlarge the vaginal opening).
-
Anal Intercourse: Rough or vigorous anal intercourse can cause trauma to the anal canal and increase the risk of developing anal fissures, particularly if adequate lubrication is not used.
-
Inflammatory Bowel Disease (IBD): Inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis can cause inflammation and ulceration of the lining of the digestive tract, including the anal canal, increasing the risk of anal fissures.
Symptoms of Anal Fissures:
The symptoms of anal fissures can vary in severity and duration but typically include:
-
Anal Pain: Pain or discomfort in the anal region, particularly during or after bowel movements, is a common symptom of anal fissures. The pain may be sharp, burning, or throbbing and may last for several hours after defecation.
-
Rectal Bleeding: Bright red blood on toilet paper, in the toilet bowl, or on stool surfaces after bowel movements is a common symptom of anal fissures. The bleeding is typically minor and may occur intermittently with bowel movements.
-
Anal Itching: Itching or irritation around the anus, often accompanied by a sensation of burning or discomfort, may occur due to exposure to fecal matter, moisture, or irritants in the anal area.
-
Burning Sensation: A burning sensation or feeling of heat in the anal region, particularly during or after bowel movements, may occur due to irritation of the anal fissure and surrounding tissue.
-
Spasm of Anal Sphincter: In some cases, the anal sphincter muscle may go into spasm (anal hypertonia) in response to the presence of an anal fissure, causing increased pain and discomfort during bowel movements.
Diagnosis and Treatment of Anal Fissures:
Diagnosis of anal fissures is typically based on a combination of medical history, physical examination, and evaluation of symptoms. Diagnostic tests such as anoscopy or sigmoidoscopy may be performed to visualize the anal canal and confirm the presence of an anal fissure.
Treatment of anal fissures aims to relieve symptoms, promote healing, and prevent recurrence. Treatment options may include:
-
Topical Medications:
- Topical Anesthetics: Over-the-counter or prescription topical anesthetic ointments or creams containing ingredients such as lidocaine or pramoxine may be applied to the anal area to provide temporary relief of pain or discomfort associated with anal fissures.
- Topical Nitroglycerin: Topical nitroglycerin ointment or cream may be prescribed to promote relaxation of the anal sphincter muscle, increase blood flow to the anal area, and facilitate healing of anal fissures.
- Topical Calcium Channel Blockers: Topical calcium channel blocker medications such as diltiazem or nifedipine may be prescribed to relax the anal sphincter muscle and promote healing of anal fissures by increasing blood flow to the affected area.
-
Dietary and Lifestyle Modifications:
- High-Fiber Diet: Increasing dietary fiber intake through fruits, vegetables, whole grains, and fiber supplements can help soften stools, promote regular bowel movements, and reduce the risk of constipation and straining during bowel movements.
- Hydration: Adequate hydration with water or other non-caffeinated fluids can help soften stools and prevent dehydration, facilitating bowel movements and reducing the risk of constipation and anal fissures.
- Stool Softeners: Over-the-counter stool softeners or laxatives may be used to help soften stools and relieve constipation, reducing the risk of straining and exacerbating anal fissures.
-
Sitz Baths: Warm sitz baths (soaking the anal area in warm water) for 10-15 minutes several times a day can help soothe irritation, reduce inflammation, and promote healing of anal fissures. Adding ingredients such as Epsom salts or baking soda to the sitz bath water may provide additional relief.
-
Botulinum Toxin Injection: In cases of chronic anal fissures that do not respond to conservative treatments, injection of botulinum toxin (Botox) into the anal sphincter muscle may be performed to relax the muscle, reduce anal pressure, and promote healing of the fissure.
-
Lateral Internal Sphincterotomy: In cases of chronic or refractory anal fissures that do not respond to conservative treatments, surgical intervention such as lateral internal sphincterotomy may be performed under anesthesia to cut a portion of the anal sphincter muscle, relieving anal pressure and promoting healing of the fissure.